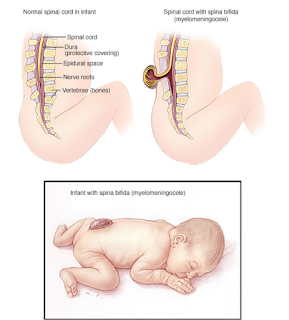
Spina bifida (myelomeningocele)
Spina bifida is a birth defect that occurs when the spine and spinal cord don't form properly. It falls under the broader category of neural tube defects. The neural tube is the embryonic structure that eventually develops into the baby's brain and spinal cord and the tissues that enclose them.
Normally, the neural tube forms early in pregnancy, and it closes by the 28th day after conception. In babies with spina bifida, a portion of the neural tube fails to develop or close properly, causing defects in the spinal cord and in the bones of the spine.
Spina bifida can range from mild to severe, depending on the type of defect, size, location and complications. When early treatment for spina bifida is necessary, it's done surgically, although such treatment doesn't always completely resolve the problem.
Types
Spina bifida can occur in different forms: spina bifida occulta, meningocele (muh-NING-go-seel) or myelomeningocele (my-uh-lo-muh-NING-go-seel). The severity of spina bifida depends on the type, size, location and complications.
Spina bifida occulta
"Occulta" means hidden. The mildest form, spina bifida occulta results in a small separation or gap in one or more of the bones of the spine (vertebrae). Many people who have spina bifida occulta don't even know it, unless the condition is discovered during an imaging test done for unrelated reasons.
Meningocele
In a form of spina bifida called meningocele, the protective membranes around the spinal cord (meninges) push out through the opening in the vertebrae, forming a sac filled with fluid. But this sac doesn't include the spinal cord, so nerve damage is less likely, though later complications are possible.
Myelomeningocele
Also known as open spina bifida, myelomeningocele is the most severe form. The spinal canal is open along several vertebrae in the lower or middle back. The membranes and spinal nerves push through this opening at birth, forming a sac on the baby's back, typically exposing tissues and nerves. This makes the baby prone to life-threatening infections.
Symptoms
Signs and symptoms of spina bifida vary by type and severity. Symptoms can also differ for each person.
- Spina bifida occulta. Because the spinal nerves usually aren't involved, typically there are no signs or symptoms. But visible indications can sometimes be seen on the newborn's skin above the spinal defect, including an abnormal tuft of hair, or a small dimple or birthmark.
- Meningocele. The membranes around the spinal cord push out through an opening in the vertebrae, forming a sac filled with fluid, but this sac doesn't include the spinal cord.
- Myelomeningocele. In this severe form of spina bifida:
- The spinal canal remains open along several vertebrae in the lower or middle back.
- Both the membranes and the spinal cord or nerves protrude at birth, forming a sac.
- Tissues and nerves usually are exposed, though sometimes skin covers the sac.
Causes
Doctors aren't certain what causes spina bifida. As with many other problems, it appears to result from a combination of genetic and environmental risk factors, such as a family history of neural tube defects and folate deficiency.
Risk factors
Spina bifida is more common among whites and Hispanics, and females are affected more often than males. Although doctors and researchers don't know for sure why spina bifida occurs, they have identified some risk factors:
- Folate deficiency. Folate (vitamin B-9) is important to the healthy development of a baby. Folate is the natural form of vitamin B-9. The synthetic form, found in supplements and fortified foods, is called folic acid. A folate deficiency increases the risk of spina bifida and other neural tube defects.
- Family history of neural tube defects. Couples who've had one child with a neural tube defect have a slightly higher chance of having another baby with the same defect. That risk increases if two previous children have been affected by the condition. In addition, a woman who was born with a neural tube defect has a greater chance of giving birth to a child with spina bifida. However, most babies with spina bifida are born to parents with no known family history of the condition.
- Some medications. For example, anti-seizure medications, such as valproic acid (Depakene), seem to cause neural tube defects when taken during pregnancy, possibly because they interfere with the body's ability to use folate and folic acid.
- Diabetes. Women with diabetes who don't control their blood sugar well have a higher risk of having a baby with spina bifida.
- Obesity. Pre-pregnancy obesity is associated with an increased risk of neural tube birth defects, including spina bifida.
- Increased body temperature. Some evidence suggests that increased body temperature (hyperthermia) in the early weeks of pregnancy may increase the risk of spina bifida. Elevating your core body temperature, due to fever or the use of saunas or hot tubs, has been associated with a possible slight increased risk of spina bifida.
If you have known risk factors for spina bifida, talk with your doctor to determine if you need a larger dose or prescription dose of folic acid, even before a pregnancy begins.
If you take medications, tell your doctor. Some medications can be adjusted to diminish the potential risk of spina bifida, if plans are made ahead of time.
Complications
Spina bifida may cause minimal symptoms or only minor physical disabilities. If the spina bifida is severe, sometimes it leads to more significant physical disabilities. Severity is affected by:
- The size and location of the neural tube defect
- Whether skin covers the affected area
- Which spinal nerves come out of the affected area of the spinal cord
This list of possible complications may seem overwhelming, but not all children with spina bifida get all these complications. And these conditions can be treated.
- Walking and mobility problems. The nerves that control the leg muscles don't work properly below the area of the spina bifida defect, causing muscle weakness of the legs, sometimes involving paralysis. Whether a child can walk typically depends on where the defect is, its size, and the care received before and after birth.
- Orthopedic complications. Children with myelomeningocele can have a variety of problems in the legs and spine because of weak muscles in the legs and back. The types of problems depend on the level of the defect. Possible problems include a curved spine (scoliosis), abnormal growth or dislocation of the hip, bone and joint deformities, muscle contractures and other orthopedic concerns.
- Bowel and bladder problems. Nerves that supply the bladder and bowels usually don't work properly when children have myelomeningocele. This is because the nerves that supply the bowel and bladder come from the lowest level of the spinal cord.
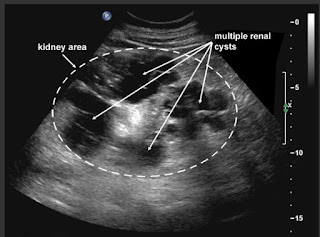
- Accumulation of fluid in the brain (hydrocephalus). Babies born with myelomeningocele commonly experience accumulation of fluid in the brain, a condition known as hydrocephalus.
- Shunt malfunction. Shunts can stop working or become infected. Warning signs may vary. Some of the warning signs of a shunt that isn't working include headaches, vomiting, sleepiness, irritability, swelling or redness along the shunt, confusion, changes in the eyes (fixed downward gaze), trouble feeding, or seizures.
- Chiari malformation type II. Chiari malformation (kee-AH-ree mal-for-MAY-shun) type II is a common brain abnormality in children with the myelomeningocele form of spina bifida. The brainstem, or lowest part of the brain above the spinal cord, is elongated and positioned lower than usual. This can cause problems with breathing and swallowing. Rarely, compression on this area of the brain occurs and surgery is needed to relieve the pressure.
- Infection in the tissues surrounding the brain (meningitis). Some babies with myelomeningocele may develop meningitis, an infection in the tissues surrounding the brain. This potentially life-threatening infection may cause brain injury.
- Tethered spinal cord. Tethered spinal cord results when the spinal nerves become bound to the scar where the defect was closed surgically, making the spinal cord less able to grow as the child grows. This progressive tethering can cause loss of muscle function to the legs, bowel or bladder. Surgery can limit the degree of disability.
- Sleep-disordered breathing. Both children and adults with spina bifida, particularly myelomeningocele, may have sleep apnea or other sleep disorders. Assessment for a sleep disorder in those with myelomeningocele helps detect sleep-disordered breathing, such as sleep apnea, which warrants treatment to improve health and quality of life.
- Skin problems. Children with spina bifida may get wounds on their feet, legs, buttocks or back. They can't feel when they get a blister or sore. Sores or blisters can turn into deep wounds or foot infections that are hard to treat. Children with myelomeningocele have a higher risk of wound problems in casts.
- Latex allergy. Children with spina bifida have a higher risk of latex allergy, an allergic reaction to natural rubber or latex products. Latex allergy may cause rash, sneezing, itching, watery eyes and a runny nose. It can also cause anaphylaxis, a potentially life-threatening condition in which swelling of the face and airways can make breathing difficult. So it's best to use latex-free gloves and equipment at delivery time and when caring for a child with spina bifida.
- Other complications. More problems may arise as children with spina bifida get older, such as urinary tract infections, gastrointestinal (GI) disorders and depression. Children with myelomeningocele may develop learning disabilities, such as problems paying attention, and difficulty learning reading and math.


Comments